If you’re curious about what is pelviacetabular surgery, you’re in the right place. This guide will take you through everything you need to know. We’ll explore what this surgery involves and its crucial role in treating hip and pelvic injuries. Having the right knowledge about each phase—from diagnosis to recovery—can help patients and their families feel more at ease. Understanding the process ensures you’re better prepared for what’s ahead.
Understanding Pelviacetabular Fractures and Surgical Options
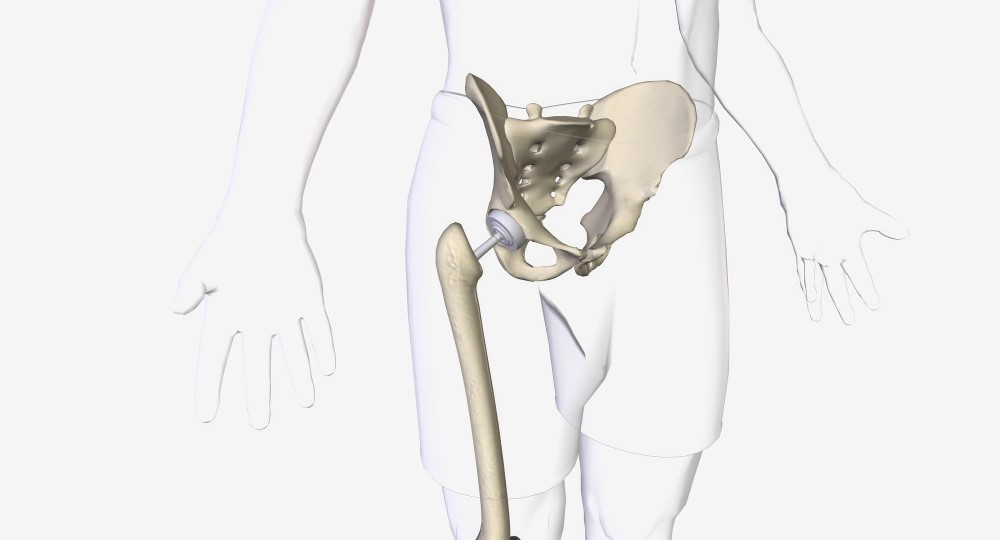
Let’s start with the basics. The pelvis is the sturdy bone structure at the base of your spine, while the acetabulum is the part of the pelvis where the head of the thigh bone joins, forming the hip joint. Accidents like falls or car crashes can cause fractures here, leading to pain and trouble walking.
Symptoms of Pelviacetabular Fractures: – Severe pain in the hip or groin area. – Difficulty or inability to walk or bear weight.
Before diving into surgical options, a proper diagnosis is crucial. Doctors usually perform physical exams and order imaging tests, like X-rays or CT scans, to get a clear picture inside your body. This precise detection paves the way for a better outcome.
When it comes to treating these fractures, surgery is often needed. Pelviacetabular surgery can involve various techniques: 1. Open Reduction and Internal Fixation (ORIF): This common approach involves repositioning bones and securing them with plates and screws. 2. Pelvic Osteotomy: Used in complex cases to reshape and stabilize the pelvis. 3. External Fixation: Provides stability during healing, using screws or rods outside the body.
With pelviacetabular surgery procedure, choosing the right technique largely depends on the fracture’s nature and the patient’s condition.
Preparing for Pelviacetabular Surgery and Understanding the Procedure
Getting ready for surgery can be a stressful time, but preparation helps ease the process. It starts with necessary medical exams to ensure your body is ready. You’ll likely talk with your doctor about potential risks. Mental and physical preparation can make a big difference in how you handle the experience.
Knowing what happens during pelviacetabular surgery is also helpful. Typically, it involves making incisions to access the broken bones. Surgeons then realign these bones to their natural positions. They stabilize the joint using screws, plates, or even external devices.
During complex procedures like pelvic osteotomies, the surgeon might take additional steps for reshaping structures. The goal is always a stable and functional joint.
Understanding these steps can remove some uncertainty, allowing you to focus on healing and recovery.
Navigating Recovery and Outlook After Pelviacetabular Surgery
Recovery is just as important as the surgery itself. Initially, you might stay in the hospital for monitoring and pain management. Medical teams keep an eye on recovery to ensure everything proceeds smoothly.
Early movement is crucial. It helps in regaining strength and mobility. Physical therapy plays a significant role here. It focuses on exercises designed to strengthen muscles and improve movement.
Recovery Tips: – Follow your doctor’s instructions closely. – Engage in regular but gentle physical therapy sessions. – Conduct home exercises as advised by health professionals.
There can be some complications of pelviacetabular surgery. Infections or blood clots are some risks, but they can be manageable with proper care and early detection. Keeping your joint healthy and active is key to a successful recovery.
Understanding the pelviacetabular surgery success rate can reassure you. Many patients return to their normal activities in due time, experiencing fewer symptoms after recovery.
By the end of this journey, having a clear picture of what is pelviacetabular surgery and knowing what to expect can empower you or your loved ones. From gaining insight into the diagnosis to navigating through recovery, every step is important for healing well. Good communication with your healthcare provider adds clarity, helping you confidently face each phase.
In summary, benefits of pelviacetabular surgery include improved mobility and reduced pain. With proper preparation for pelviacetabular surgery and understanding the procedure, recovery can be smooth. Stay informed, ask questions, and follow your care team’s advice to enhance your recovery process.
Feel assured in knowing that these efforts aim to improve your quality of life, helping you return to daily activities with strength and confidence.